

 Article
Article

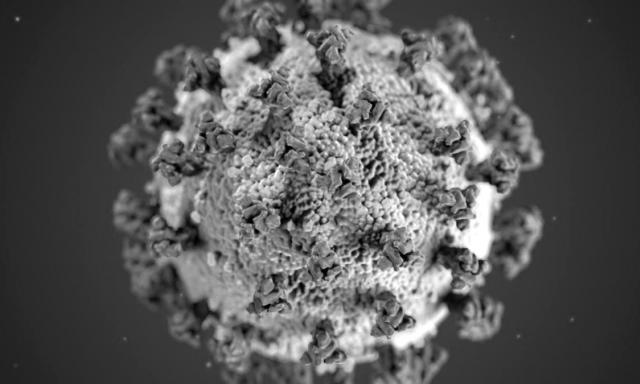
 The coronavirus has spread around the world rapidly. Here, one Darden professor examines the financial implications versus the ethical ones. What would an uncontrolled outbreak mean in the U.S.? What can we learn from China and Italy? And what questions should organizations be asking?
The coronavirus has spread around the world rapidly. Here, one Darden professor examines the financial implications versus the ethical ones. What would an uncontrolled outbreak mean in the U.S.? What can we learn from China and Italy? And what questions should organizations be asking?
Insights from
Organizations around the world are working through how to respond to the novel coronavirus, posing one of the greatest challenges to leaders in a long time. Do they restrict travel? Doing so would have substantial financial implication, make months of preparation worthless and lower the morale of many stakeholders who enjoy travel. However, travel is what brought the coronavirus to the country in the first place — and what continues to spread it to new communities within the country.
What about instituting remote work procedures? In-person meetings and events may be a critical part of an organization’s activities and an important part of the value it offers. Perhaps there are no known cases of the virus in a given community. However, once it does gain a foothold, social distancing is the only way to slow the spread. Carriers of the virus may unwittingly spread it for days before symptoms manifest themselves.
Above all, one of the greatest challenges is to balance an organization’s economic concerns with the question of what is ethically the best course of action.
The novel coronavirus was first identified in Wuhan, China, in December 2019. It jumped from bats via an intermediate host (most likely pangolins) that was traded in live animal markets to humans. The virus has officially been named “SARS-CoV-2,” and the disease that it causes has been named “coronavirus disease 2019” (abbreviated “COVID-19”). It spreads among humans via respiratory droplets from coughing as well as by touching infected surfaces. In an uncontrolled outbreak, the disease burden grows exponentially, with cases doubling approximately every six days. The incubation period, i.e. the time between when one is exposed to the virus and when one develops symptoms of disease, is from two to 14 days, with an average of five days. Those infected usually present with a fever, a dry cough and general fatigue, frequently involving a mild form of pneumonia. About 15–20 percent of cases develop more severe pneumonia that requires hospitalization, intensive care, and in many cases, mechanical ventilation. The latest World Health Organization estimate of the fatality rate is 3.4 percent.
Some may argue that it’s up to individuals how much risk they’re willing to take. But becoming infected affects not only yourself but also endangers others, as infected individuals can spread the disease and expose their community to the substantial risks involved, up to and including premature death. There is thus a crucial ethical component to the public health precautions that individuals and organizations take. Economists call this public health aspect of infectious diseases an externality — i.e., an effect on others that an individual or organization that only cares about their own well-being is tempted to ignore. (A typical example of another type of externality is pollution — when an individual pollutes, society as a whole suffers.) When an individual spreads the disease it does not impose any cost on them, but costs the newly infected dearly. In fact, the externalities of infectious diseases come in two forms: healthy people not taking sufficient precaution to avoid becoming infected (because they do not internalize the risks this will create for others) and exposed people not taking sufficient precaution to avoid spreading the disease.
Others may challenge the idea of whether to try to contain the virus at all. The disease seems unstoppable — it has spread around the world in a matter of weeks. Why go to such extreme lengths and incur enormous economic costs to try to prevent the unpreventable? Aren’t we all just caught up in a bad case of mass hysteria that is even more infectious — and pernicious — than the coronavirus itself? However, that argument neglects all the lives at risk and the extent to which an uncontrolled outbreak risks overwhelming medical resources and exacerbating the ultimate death toll.
What adds to the challenge on how to respond is the highly disproportionate impact of the disease on different people. The elderly and those with pre-existing conditions are at much greater risk of death from COVID-19 than others. For example, taking into account all the risk factors, a male in his 70s with a heart condition who contracts the virus has a risk of death that is significantly higher – perhaps in excess of 25 percent. (Useful information on mortality rate by demographics can be found on world statistics site Worldometer.)
The experience of regions that have dealt with large outbreaks of COVID-19 in recent weeks, chiefly Wuhan and northern Italy, suggest two lessons.
Organizations need to determine how to answer the following questions:
The epidemiological realities of the disease have stark implications for organizations. Decisions made now will determine the way that stakeholders will work, travel and interact with each other in coming weeks and months, and it will determine the economic losses companies will experience. And as much as the virus will affect organizations, those organizations’ reaction to it will have a crucial effect on how fast and how widely COVID-19 will spread in their communities, and how many lives will be lost to the disease. This adds a crucial ethical component to the trade-off. Balancing the economic fall-out with this ethical dimension is the most significant leadership challenge of our time.
An expert in macroeconomics, artificial intelligence, financial stability and international finance, Korinek currently researches the implications of AI for business, the economy and the future of work. His work has been featured in top journals and the mainstream media, including The Economist, The Wall Street Journal and Bloomberg.
In addition to serving as associate professor at both UVA’s Darden School of Business and Department of Economics, Korinek is a Research Associate at the National Bureau of Economic Research. Prior to his UVA appointments, he held positions at the University of Maryland as well as Johns Hopkins University, and he was a visiting scholar at Harvard University, the International Monetary Fund and the World Bank.
M.A., University of Vienna; Ph.D., Columbia University
The Coronavirus and Managing Your Organization’s Response
Share